Driving Excellence in Healthcare
Helping You Develop Continuous Quality Improvement Strategies
At Ascend Technologies, we understand the critical role that quality plays in the healthcare industry. Our comprehensive services are designed to help healthcare organizations develop and implement strategic quality initiatives that drive excellence and improve patient outcomes. With our expertise and tailored solutions, we empower healthcare providers to achieve their quality goals and deliver exceptional care.
ascend’s Structured Approach
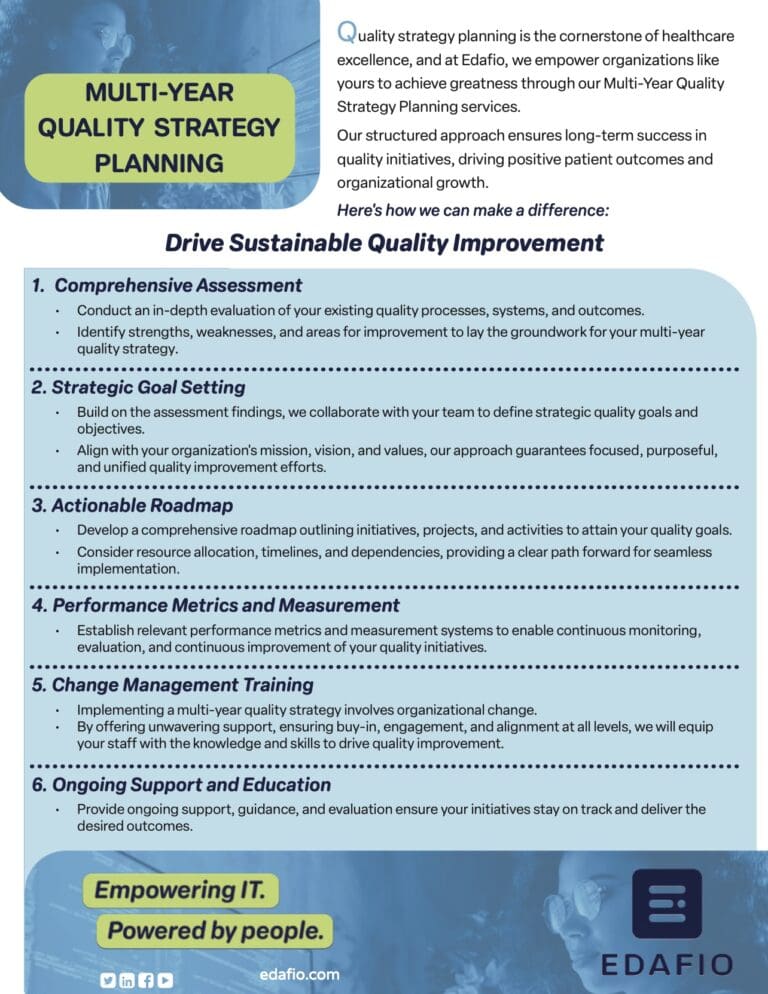
Effective quality strategy planning is key to achieving excellence in healthcare. Edafio’s Multi-Year Quality Strategy Planning services offer a structured approach to develop and implement long-term quality initiatives. We can help by offering:

Comprehensive Assessment
Our experienced consultants perform a thorough assessment of your current quality processes, systems, and outcomes. We identify strengths, weaknesses, and opportunities for improvement, serving as the foundation for your multi-year quality strategy.
Strategic Goal Setting
Based on the assessment findings, we work collaboratively with your team to define strategic quality goals and objectives. These goals are aligned with your organization’s mission, vision, and values, ensuring a clear and focused direction for quality improvement efforts.
Actionable Roadmap
We develop a comprehensive roadmap that outlines the initiatives, projects, and activities needed to achieve your quality goals. This roadmap considers resource allocation, timelines, and dependencies, providing a clear path forward for successful implementation.
Performance Metrics and Measurement
To track progress and success, we assist in establishing relevant performance metrics and measurement systems. These metrics enable ongoing monitoring, evaluation, and continuous improvement of your quality initiatives.
Change Management and Training
We understand that implementing a multi-year quality strategy involves organizational change. Our change management experts support your team in navigating the transformation process, ensuring buy-in, engagement, and alignment at all levels. We also provide training programs to equip your staff with the necessary knowledge and skills to drive quality improvement.
Ongoing Support and Evaluation
Ascend is your dedicated partner throughout the multi-year quality strategy planning journey. We provide ongoing support, guidance, and evaluation to ensure that your initiatives stay on track and deliver the desired outcomes.

Why Choose Ascend for Multi-Year Quality Strategy Planning?
Partnering with Ascend for your Multi-Year Quality Strategy Planning offers several compelling advantages, including:
Healthcare Expertise
Ascend has deep industry knowledge and expertise in healthcare. We understand the unique challenges and regulatory requirements faced by healthcare organizations, allowing us to tailor our solutions to your specific needs.
Collaborative Approach
We believe in working closely with your team to develop a multi-year quality strategy that reflects your organizational goals and values. Our collaborative approach ensures that your initiatives are aligned with your vision and have the support of key stakeholders.
Proven Methodologies
Ascend utilizes proven methodologies and best practices in quality improvement. Our consultants bring a wealth of experience in driving successful quality initiatives, giving you the confidence that your strategic planning is in capable hands.
Tailored Solutions
We recognize that every healthcare organization is unique. Our solutions are customized to address your specific challenges and opportunities, providing a roadmap that aligns with your resources, timelines, and budget.
Focus on Patient Outcomes
At Ascend, we are committed to improving patient outcomes. Our multi-year quality strategy planning services are designed to enhance the quality of care you provide, resulting in better patient experiences and improved health outcomes.
Frequently Asked Questions
How does Ascend set strategic quality goals and objectives for my organization?
Based on the assessment findings, we collaborate with your team to define strategic quality goals and objectives. These goals are aligned with your organization’s mission, vision, and values, ensuring a clear and focused direction for quality improvement efforts.
What can I expect from the actionable roadmap provided by Ascend?
The actionable roadmap developed by Ascend outlines the initiatives, projects, and activities required to achieve your quality goals. It considers resource allocation, timelines, and dependencies, providing a clear path forward for successful implementation.
How does Ascend establish performance metrics and measurement systems for quality improvement?
We assist in establishing relevant performance metrics and measurement systems to track the progress and success of your quality initiatives. These metrics enable ongoing monitoring, evaluation, and continuous improvement.
How can Ascend’s change management support benefit my organization during the strategic planning process?
Implementing a multi-year quality strategy involves organizational change. Ascend’s change management experts support your team in navigating the transformation process, ensuring buy-in, engagement, and alignment at all levels. We also provide training programs to equip your staff with the necessary knowledge and skills to drive quality improvement.
What ongoing support does Ascend provide during the multi-year quality strategy planning journey?
Ascend remains your dedicated partner throughout the multi-year quality strategy planning journey. We offer ongoing support, guidance, and evaluation to ensure that your initiatives stay on track and deliver the desired outcomes.
How does Ascend customize its Multi-Year Quality Strategy Planning services to fit my organization’s needs?
At Ascend, we understand that every healthcare organization is unique. Our solutions are customized to address your specific challenges and opportunities, providing a roadmap that aligns with your resources, timelines, and budget.
How can I benefit from Ascend’s healthcare expertise during the planning process?
Ascend has in-depth knowledge and experience in the healthcare industry, allowing us to understand the unique challenges and regulatory requirements faced by healthcare organizations. This expertise ensures that our strategic planning solutions are well-suited to your organization’s needs.
free Download: Multi-Year Quality Strategy Planning Overview
Quality strategy planning is the cornerstone of healthcare excellence, and at Ascend, we empower organizations like yours to achieve greatness through our Multi-Year Quality Strategy Planning services. Our structured approach ensures long-term success in quality initiatives, driving positive patient outcomes and organizational growth.
Leverage Your Full Potential Today
Contact Ascend today to learn more about how we can drive excellence in your healthcare organization. Let us be your trusted partner in developing and implementing a strategic quality roadmap that transforms your care delivery and elevates patient outcomes.





